By Pamela Maragliano-Muniz, BSDH, DMD
As dental professionals, we evaluate our patients on a routine basis and continually provide strategies to prevent dental caries. These strategies include caries risk assessment1 and individualized risk management recommendations. There is an abundance of products on the market and it can be challenging for dental professionals to hone their recommendations. In general, caries management programs receive criticism for being time consuming and complicated for private practices. It is essential to streamline and simplify2 caries management for the private practice it can be practiced routinely and indefinitely. The purpose of this article is to discuss simple strategies to get the maximum impact of caries management within the private practice.

Getting Started
Before implementing a caries management program, it is vital for the dental or dental hygiene practice to plan and organize as a team. A few items for consideration include:
- Understanding the caries process. It is essential to become educated in the caries process so that risk assessment and risk management can be tailored for each individual practice.
- Caries risk assessment. Which team member will provide risk assessment? How will risk be assessed; will a questionnaire be used or will caries risk be assessed using another method?
- Caries risk management. Who will make risk management recommendations? How will this information be conveyed, verbally or via handouts?
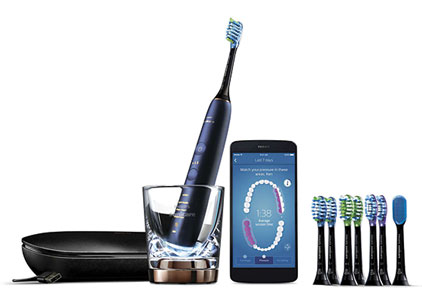
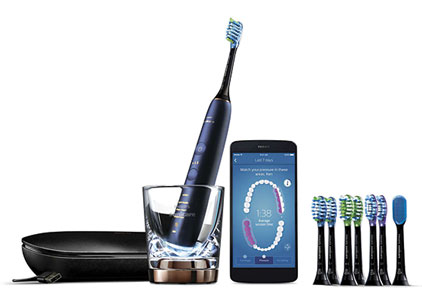
- Product recommendations. It is important to decide which products will be recommended for patients in each risk category, including toothbrushes, interdental cleaning strategies and topical pastes.
- Documentation. Documenting caries risk assessment, caries risk category assignment, risk management recommendations and patient’s acceptance of your recommendations is essential. Custom documentation templates within the electronic health record are particularly useful to calibrate different members of the dental team.
The Caries Process
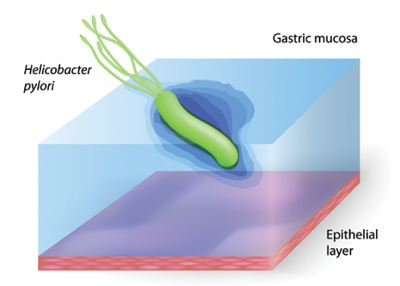
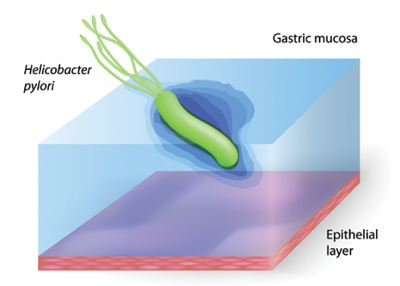
Historically, dental caries was thought to be the result of the interaction of a susceptible tooth, fermentable carbohydrates and time.3 Later research uncovered that the progression of dental caries is multifactorial4 is significantly more complex5. Dental caries is the result of an oral environment that is conducive to the progressive demineralization of the hard structures in the oral cavity. This net loss of tooth mineral is due, in part, to the proliferation of cariogenic bacteria that thrive in a low-pH (acidic) environment.6

 The study can be found here. This study shows many limitations, including the sample time, lack of information about iodine in salt, which could modify associations between fluoride and cognition, and the lack of data on fluoride content in water given that determination of fluoride content.(1) Therefore, the study has no way of knowing how much fluoride the women were exposed to via natural fluoride in their water source. Determining the source of the water is important because natural fluoride in the water source has up to 1.38 mg/L, which is double of that of the United States.(1) Furthermore, we have no idea which women drank from the water source vs. the bottled water.
The study can be found here. This study shows many limitations, including the sample time, lack of information about iodine in salt, which could modify associations between fluoride and cognition, and the lack of data on fluoride content in water given that determination of fluoride content.(1) Therefore, the study has no way of knowing how much fluoride the women were exposed to via natural fluoride in their water source. Determining the source of the water is important because natural fluoride in the water source has up to 1.38 mg/L, which is double of that of the United States.(1) Furthermore, we have no idea which women drank from the water source vs. the bottled water.