Ferris State searches for ways to initiate oral health as part of collaborative care
Jamie Freitag-Dooley, RDH, BIS, CLC
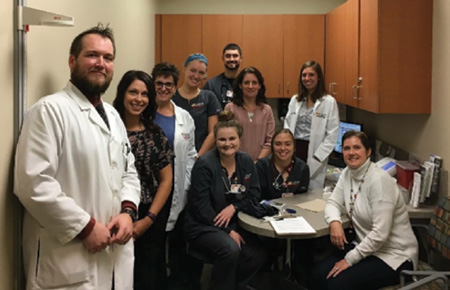
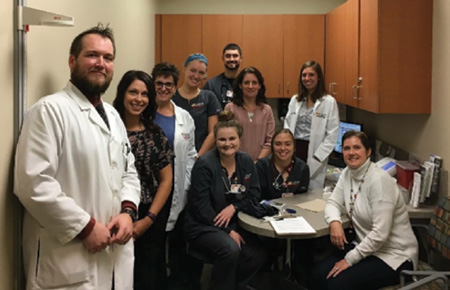
Providers and students from optometry, pharmacy, nursing, social work, and dental hygiene gather together at Ferris State University’s Interprofessional Wellness Clinic to discuss ways they can integrate oral health into an existing program that serves diabetes patients.
According to Oral Health in America: A Report from the Surgeon General, “all care providers can and should contribute to enhancing oral health.” Now that the medical community has finally embraced the oral systemic link as a care gap in their treatment, hygienists are being considered as affordable educators and disease screeners in health-care systems nationwide to improve health outcomes.
Confidence starts in school. What better place to prepare students to be part of the collaborative care model. Even so, are our dental hygiene program curriculums including this model in their teaching methods? How can current clinicians collaborate in their communities? There are exciting projects going on now that are making a difference in disease by integrating hygienists into collaborative care teams.